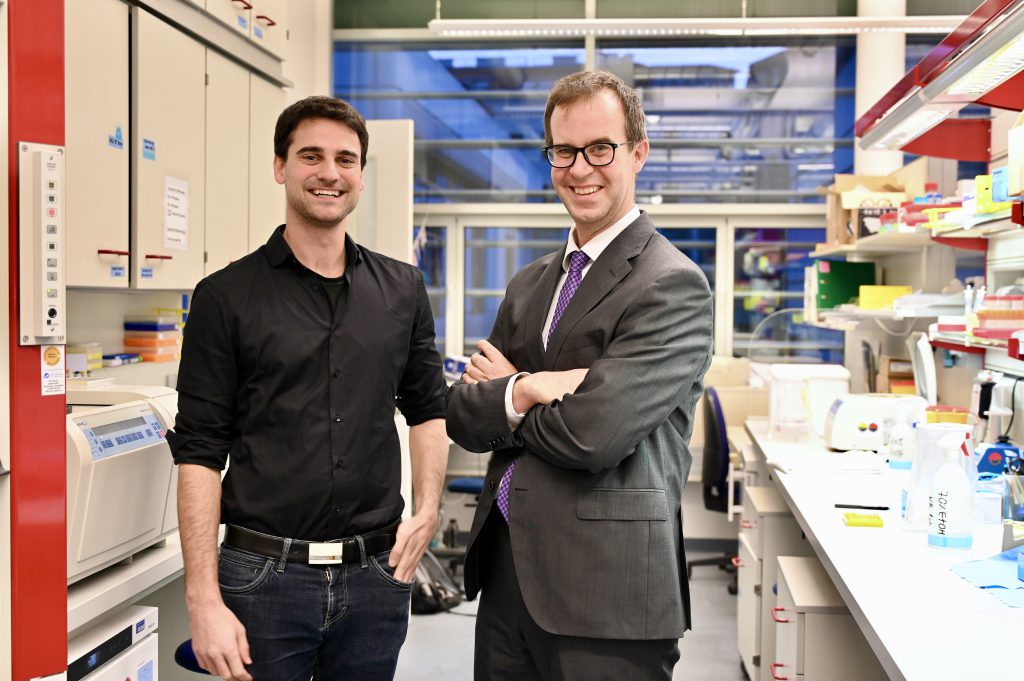
Bridging to clinical translation: Professor Kaan Boztug honored for his research on personalized medicine approaches for inborn errors of immunity
(Vienna, August 2025) Prof. Dr. med. Kaan Boztug has been awarded the prestigious Novartis Prize for Therapy-Relevant Immunological Research 2025. As a pediatrician and expert in rare diseases of the immune system and blood formation, Boztug bridges clinical practice and research in his work. This approach enables him to translate molecular insights directly into the care of young patient. A strategy that lends his scientific breakthroughs exceptional clinical relevance.
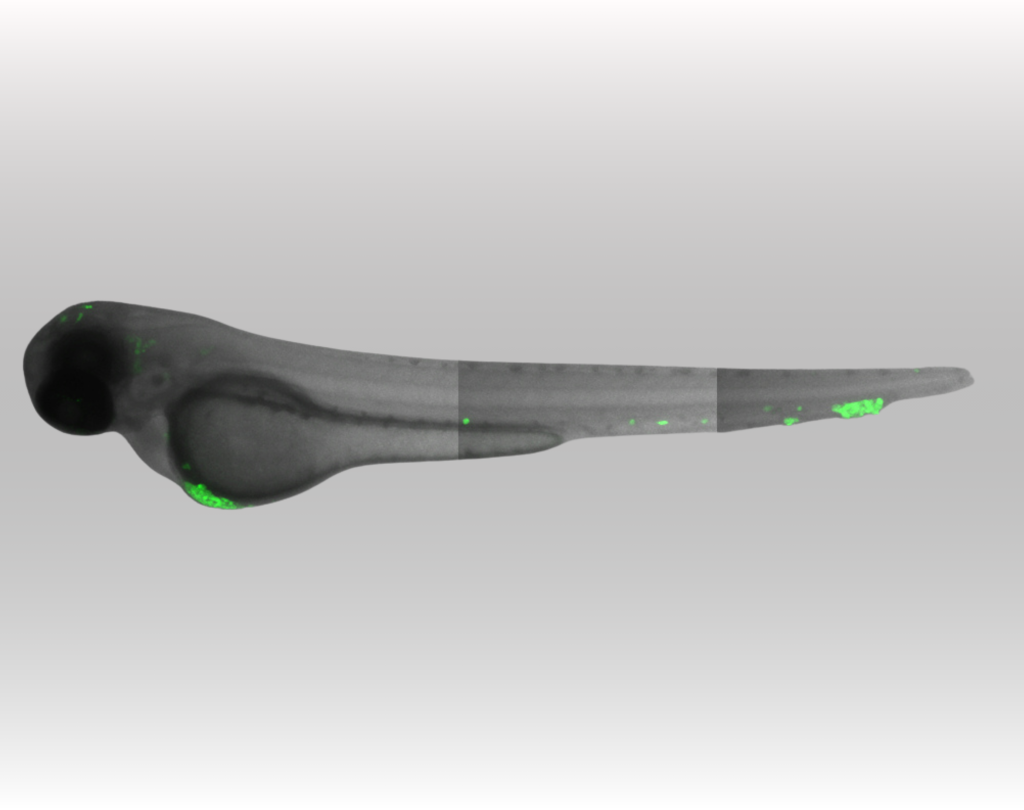
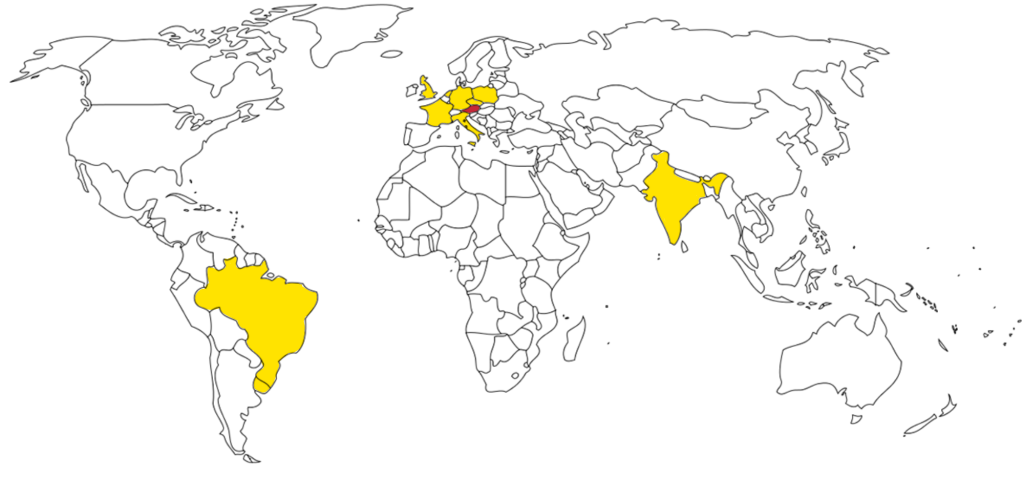
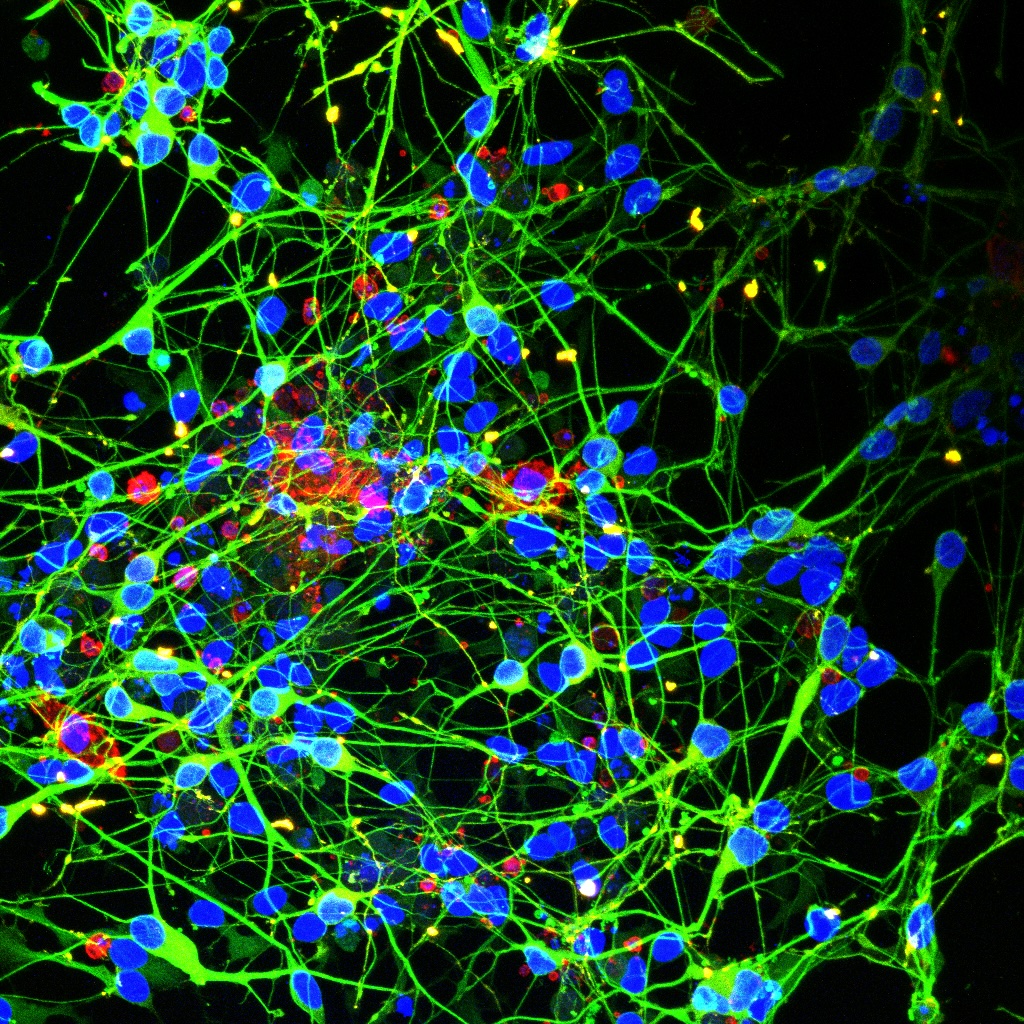
Boztug’s field of expertise is the study of inborn errors of immunity (IEI) and the elucidation of the molecular basis of inherited bone marrow failure syndromes. His research group investigates the molecular mechanisms underlying immune (dys)regulation, including autoimmunity and cancer predisposition in childhood. Boztug has played a leading role in the initial description and molecular characterization of more than 20 previously unknown diseases.
“The vision of our research team and the entire institute is to provide long-term help in the near future to those children who cannot yet be sustainably cured with existing treatment options. This aspiration shapes my work and is the driving force behind the consistent and passionate further development of our research activities,” says Boztug. Due to his dual role as a clinician and a scientist, he is particularly keen to use new scientific findings to develop new treatment options.
About Kaan Boztug
Since February 2025, Kaan Boztug has been appointed as Professor (W3) and Director of the Clinic for Pediatric Immunology and Rheumatology, and is a Principal Investigator in the ImmunoSensation Cluster of Excellence at the University Hospital Bonn, as well as Research Group Leader (formerly Scientific Director until January 2025)) at the St. Anna Children’s Cancer Research Institute in Vienna. He is also an Adjunct Principal Investigator (PI) at the CeMM Research Center for Molecular Medicine of the Austrian Academy of Sciences and a Professor of Paediatrics and Inflammation Research at the Medical University of Vienna. His work has been supported by an ERC Starting Grant (ImmunoCore, 2012–2018) and an ERC Consolidator Grant (iDysChart, 2019–2025), among others.
About the Novartis Prize for Therapy-Relevant Immunological Research
Basic research in immunology holds great potential for the development of innovative immunotherapeutic approaches. However, the successful translation of new immunological insights into clinical practice remains a major challenge and demands a high degree of interdisciplinarity. For this reason, the German Society for Immunology, in collaboration with the Novartis Foundation for Therapeutic Research, awards the Novartis Prize for Therapy-Relevant Immunological Research every two years. This €10,000 prize honors work that builds a bridge between immunological and clinical research. This year, the award is shared with another award winner, Professor. Dr. med. Evelyn Ullrich.