Childhood cancer: “New” immune system responds better to therapy
(Vienna, 9.8.2023) Scientists at St. Anna Children’s Cancer Research Institute and the Eberhard Karls University of Tübingen have shown that immunotherapy after stem cell transplantation effectively combats certain nerve tumors in children. Crucially, stem cells from a parent provide children with a new immune system that responds much better to immunotherapies. These results of an early clinical trial were published in the prestigious Journal of Clinical Oncology.
Childhood tumors of the nervous system, known as neuroblastomas, are associated with an unfavorable prognosis if the tumor is classified as a high-risk type. The chances are particularly poor for patients in the relapsed stage. In this case, immunotherapy following stem cell transplantation is now associated with long-term survival in a substantial proportion of the patients included in a recent study. Compared to an earlier study the survival rate was increased.

result in stronger and longer lasting
tumor conrol.”
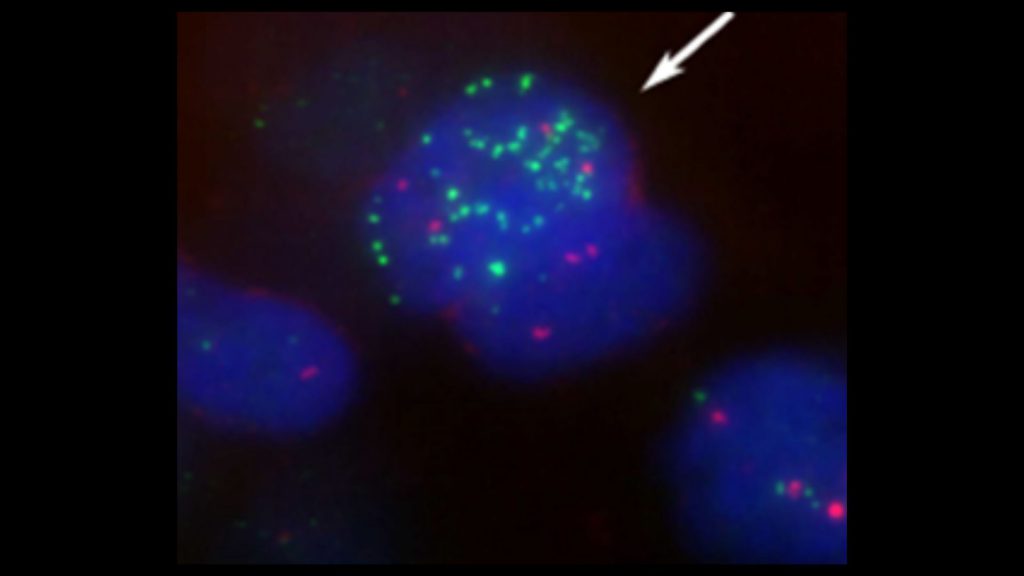
(c) Harald Eisenberger
“After the transplantation of stem cells from a parent, the patients are equipped with a new immune system. This enables a better immune response to the subsequent immunotherapy and clearly improves the outcome,” explains Prof. Ruth Ladenstein, MD, head of the Studies & Statistics group for Integrated Research and Projects (S2IRP) at St. Anna Children’s Cancer Research Institute and professor at the Department of Pediatrics and Adolescent Medicine at MedUni Vienna, who played a key role as co-first author.
Long-term survival exceeds 50 percent
“After a median follow-up of about eight years, we see that more than half of the study patients live five years or longer with their disease,” Prof. Ladenstein reports (5-year overall survival: 53%). In comparison, the 5-year overall survival in an earlier study, in which stem cell transplantation was not followed by immunotherapy, was only 23 percent. Those patients who showed a complete or partial response to prior treatment had significantly better survival.
“In summary, immunotherapy with dinutuximab beta following transplantation of stem cells from matched family donors resulted in remarkable outcomes when patients had at least a partial response to prior treatment,” says Prof. Ladenstein. “In our study, there were no unexpected side effects and the frequency of graft-versus-host-disease was low.”
Boosting natural killer cells
Dinutuximab beta is an antibody that binds to a specific molecule (GD2) on the surface of tumor cells, marking them for destruction by the immune system. Subsequently, specific immune cells, known as natural killer cells, can attack the tumor. However, prior chemotherapies may impair certain abilities of natural killer cells. “Therefore, a transplantation of intact natural killer cells from matched family donors seems reasonable before immunotherapy is administered. The transplanted, new natural killer cells are now able to target the tumor cells more efficiently – by means of an antibody-dependent reaction,” explains Prof. Ladenstein.
According to the authors, further studies are needed to determine the individual components of the therapeutic approaches. Recently, conventional chemotherapy has also been combined with immunotherapy early in the treatment strategy, resulting in similarly improved response rates. However, the hope is that the concept of a renewed immune system through a healthy parent in combination with the described transplantation procedure could further increase survival rates: “Our approach could thus result in stronger and longer lasting tumor control. A randomized study would be necessary to scientifically substantiate the additional potential benefit of a new immune system in the context of relapse therapy,” Prof. Ladenstein adds.
—
Publication
Anti-GD2 Antibody Dinutuximab Beta and Low-Dose Interleukin 2 After Haploidentical Stem-Cell Transplantation in Patients With Relapsed Neuroblastoma: A Multicenter, Phase I/II Trial
Tim Flaadt, MD*; Ruth L. Ladenstein, MD, PhD*; Martin Ebinger, MD; Holger N. Lode, MD; Helga Björk Arnardóttir, MSc; Ulrike Poetschger, PhD; Wolfgang Schwinger, MD; Roland Meisel, MD; Friedhelm R. Schuster, MD; Michaela Döring, MD; Peter F. Ambros, PhD; Manon Queudeville, MD; Jörg Fuchs, MD; Steven W. Warmann, MD; Jürgen Schäfer, MD; Christian Seitz, MD; Patrick Schlegel, MD; Ines B. Brecht, MD; Ursula Holzer, MD; Tobias Feuchtinger, MD; Thorsten Simon, MD; Johannes H. Schulte, MD; Angelika Eggert, MD; Heiko-Manuel Teltschik, MD; Toni Illhardt, MD; Rupert Handgretinger, MD#; and Peter Lang, MD#
*T.F. and R.L.L. contributed equally and share first authorship
#R.H. and P.L. shared senior authorship
J Clin Oncol 2023, June 10. https://ascopubs.org/doi/10.1200/JCO.22.01630
About high-risk neuroblastoma
Neuroblastomas are the most common pediatric solid tumors derived from nerve tissue outside the brain. High-risk neuroblastomas include patients with metastatic disease above 18 months and patients of all ages whose tumors harbor a MYCN amplification. Unfortunately, the prognosis is still unsatisfactory, with only about half of the children with high-risk neuroblastoma surviving the disease in the long-term. Current standard treatment includes chemotherapy, surgery, autologous stem cell rescue, and isotretionin in combination with immunotherapy.
Funding
The study was supported by grants from Aktion Nils and the Gesellschaft für Kinderkrebsforschung (GKKF) Geltendorf, from BILD hilft e.V.“Ein Herz für Kinder”, from the Fördergesellschaft Kinderkrebs-Neuroblastom-Forschung Baden-Baden, from the Deutsche Kinderkrebsstiftung Bonn, from the excellence cluster iFIT (gefördert durch die Deutsche Forschungsgemeinschaft (DFG) im Rahmen der Exzellenzstrategie des Bundes und der Länder), from the Dieter Schwarz Stiftung Neckarsulm, from the Reinhold-Beitlich Stiftung Tübingen, and from the Förderverein and Stiftung für krebskranke Kinder Tübingen e.V. Recloning and production of the ch14.18 monoclonal antibody were done at Polymun Scientific (Vienna, Austria) and enabled by a SIOPEN fundraising effort in 2001 and by a grant from Aktion Nils.
Press Release >>