New Insights into Risk Factors for a Subtype of Acute Lymphoblastic Leukemia
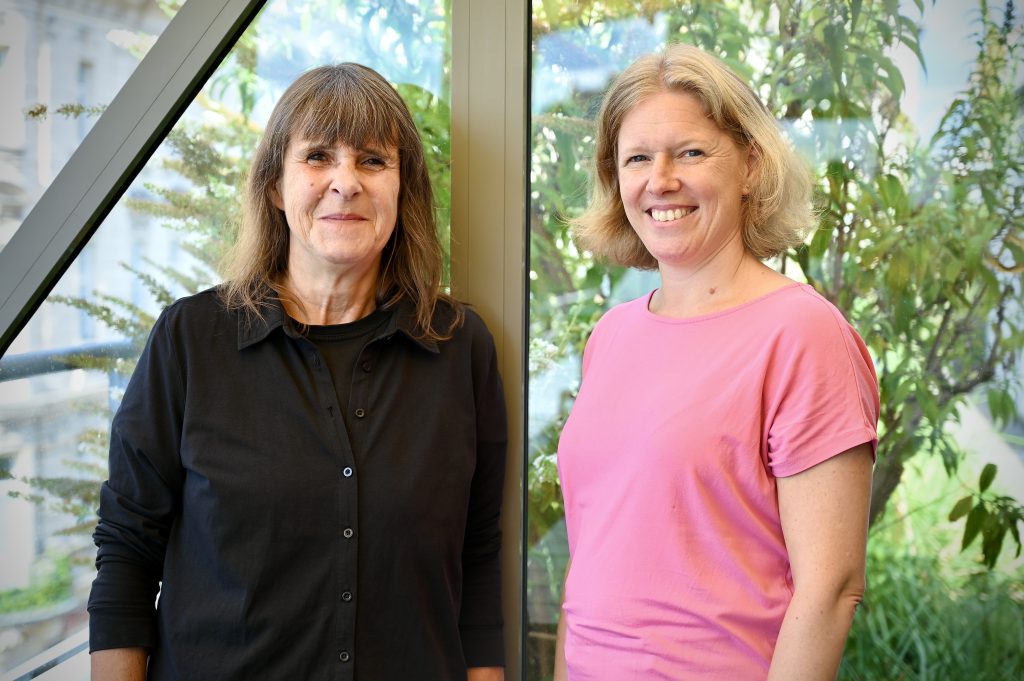
A team around Sabine Strehl and Dagmar Schinnerl has made significant progress in studying a subtype of B-cell acute lymphoblastic leukemia. The research findings, recently published in the Blood Cancer Journal, shed new light on the specific characteristics and risk factors of this form of leukemia.
B-cell acute lymphoblastic leukemia (B-ALL) is the most common cancer in children and adolescents. While it is highly treatable today, further improvement in cure rates requires a deeper understanding of the risk factors for the various subtypes of B-ALL. In a large-scale study, samples collected over more than 20 years from 1,237 patients treated in Austria according to international therapy protocols were analyzed. Seventy cases of the so-called DUX4 subtype of B-ALL were identified. This subtype is one of more than 20 subtypes of this leukemia, characterized by specific genetic and immunological features. The DUX4 subtype is marked by gene fusions leading to the overproduction of abnormal forms of the DUX4 protein, which is inactive in normal blood cells, and a typical gene expression profile. Additionally, the leukemic cells carry the surface molecule CD371.
The study results show that patients with this form of B-ALL generally have a good prognosis. The 5-year survival rate is 95.1%, and the 10-year survival rate is 88.1%. However, risk factors have been identified that may worsen the prognosis, particularly the loss of certain DNA segments (IKZF1plus deletion profile) and mutations in the tumor suppressor TP53.
Collaboration of Research, Diagnostics and Clinic
“Our research shows that the risk factors for DUX4-positive B-ALL need to be better understood to optimize therapy,” says Sabine Strehl. The comprehensive analysis of the large number of patients was conducted in collaboration with Labdia Laboratory Diagnostics GmbH, a subsidiary of St. Anna CCRI, and the St. Anna Children’s Hospital. First author Dagmar Schinnerl emphasizes, “Without the collaboration of research, diagnostics, and clinic, this work would not have been possible. We are pulling together in the same direction to further optimize the treatment of acute lymphoblastic leukemia in children and adolescents.”
In addition to the IKZF1plus deletion profile and TP53 mutations, other important results of the study relate to the so-called swALL phenotype, in which leukemia cells transform into another type of blood cell resembling monocytes during the early phase of therapy. These patients also have a poorer prognosis, requiring an adjustment in the monitoring of minimal residual disease. On the other hand, an early poor response to therapy, usually indicative of a high risk, appears to be less relevant for patients with DUX4 B-ALL.”Our findings highlight the need to revise the current prognostic factors and risk stratification parameters for DUX4 patients,” say Strehl and Schinnerl. “It is too early to make a therapy recommendation. Our data still need to be confirmed in independent studies,” the authors acknowledge, “but we provide a roadmap of what factors need to be examined in detail.”
Publication
Schinnerl D, Riebler M, Schumich A, Haslinger S, Bramböck A, Inthal A, Nykiel M, Maurer-Granofszky M, Haas OA, Pötschger U, Köhrer S, Nebral K, Dworzak MN, Attarbaschi A, Strehl S. Risk factors in DUX4-positive childhood and adolescent B-cell acute lymphoblastic leukemia. Blood Cancer J. 2024 Jul 22;14(1):119. doi: 10.1038/s41408-024-01099-3.